Does Vitamin D keep us (especially those who exercise outdoors) healthy?

By: Stephanie Boville MSc., RD
As the snow and cold weather rolls in, it is often accompanied by the common cold or worse, the flu. Endurance athletes are more at risk of illness, specifically upper respiratory tract infections (URTI) because they often engage in intense training sessions outdoors that often last over an hour and athletes who are overtrained are even more at risk. Studies show that runners training for 96km/week doubled their odds of illness compared to those training only 32km/week and about 40% of marathoners experience an URTI in the 2 months of winter training leading up to a marathon race.
Along with the vigorous training, other factors such as stress, lack of sleep and inadequate nutrition can lead to immune suppression, increasing risk of illness. Being a Registered Dietitian, I would like to explain how vitamin D may help boost your immune function this winter season.
Immune function in athletes:
There are a few reasons why URTI’s are common, although this is not a complete list of all the immunological changes that occur with heavy exercise, it will provide background as to why illness is specific to the upper respiratory system.
- Cortisol, a stress hormone, is increased which temporarily suppress the immune system.
- Specific biomarkers of inflammation increase and have been linked to immune suppression.
- Natural Killer cell (cells that kill viruses) activity is reduced for at least 6 hours by 40-60% following exercise lasting over an hour.
- Nasal neutrophil phagocytosis (cells responsible for searching for and destroying bacteria) is decreased
- Nasal and salivary Immunoglobuin A (IgA) (antibodies secreted in the saliva which are responsible for protecting the immunity of the respiratory tract) concentration is decreased by 70% for 18h after a 31km race.
- Nasal mucociliary transit time is prolonged post marathon race for several days, meaning the movement of foreign particles and bacteria out of the upper respiratory tract and away from the lungs is less efficient.
All of these aspects combined demonstrate that there is possibly a window of increased risk of contracting an URTI after exercise because the immune system is compromised. The last three points demonstrate a few possible reasons to why the upper respiratory tract is so vulnerable, especially because the nose and throat are the first line of defense against pathogens entering the body.
Nutrition and Immunity:
The first point I want to make is that overall adequate nutrition plays a role in maintaining a healthy immune system. If we look at the IOC paper discussing the consequences athletes face when they are in a relative energy deficient state (inadequate overall energy intake), we see that one of the many systems affected is immunity. Therefore, you might want to think again before you try and “shred those Christmas and New Year’s gains” in mid flu season unless absolutely necessary. We need to understand that good dietary basics are necessary to support a healthy immune system before we start to get more specific with our micronutrients.
Vitamin D and Immunity:
There are three studies I want to discuss:
Study 1:
Study 1 was an observational study investigating the effects of vitamin D status on the incidence and immune function during winter training in 239 endurance athletes. They found that being vitamin D deficient resulted in significantly more symptom days and increased symptom severity of URTI when compared to optimal, adequate and inadequate vitamin D levels. They also investigated saliva samples which showed that salivary IgA concentration was significantly reduced in athletes with deficient levels of vitamin D, and that athletes with adequate, inadequate and deficient levels of vitamin D had reduced salivary IgA secretion rates compared to optimal levels. From the information in the paragraphs about we see that one area in common, the salivary IgA. Both exercise and reduced levels of vitamin D results in decreased salivary IgA concentration and secretion rates which suggests that having an optimal levels of vitamin D has an important role to play in maintaining immunity in athletes. Lastly this study found that the antimicrobial peptides in the blood were positively correlated with vitamin D status suggesting that optimal vitamin D may result in better immune function and protection.
One limitations of this study is that it was an observational study and therefore no clear links can be determined whether an intervention with vitamin D supplement in vitamin D deficient athletes will reduce frequency, length and severity of illness. Rather this study concludes that there is an association between reduced vitamin D status and increased illness length and severity along with reductions in immunological markers.
Study 2:
Study 2 investigated the effect of a 2000IU vitamin D supplement on length and severity of URTI in non-athletic adults. They supplemented participants for 12 weeks with Vitamin D or placebo and found no differences in URTI incident or severity. However, there are a few things to consider. First, we know athletes have a higher risk of URTI’s, and therefore the results may not be generalizable to an athletic population. Second, even though there was a significant increase in Vitamin D levels with supplementation it was not enough to get participants to an “optimal” level as set out by study 1 and vitamin D levels may not have been sufficient enough to show changes in immunity. Third, both groups had adequate baseline levels of vitamin D and it could be possible immune function is only compromised at inadequate or deficient levels of vitamin D. Fourth they did not do any salivary or plasma samples and therefore we can not see the immunological changes.
Study 3:
Study 3 investigated the effects of 14 weeks of 5000IU vitamin D3 supplements in 39 athletes on antimicrobial peptides and proteins. They found that the 5000IU dose for 14 weeks was enough to elevate blood levels of vitamin D to optimal levels and that 14 weeks of winter training without supplementation decreased vitamin D levels. 5000 IU of vitamin D per day resulted in significantly higher percent change in antimicrobial peptide concentration compared to placebo and increased the salivary IgA and antimicrobial peptide secretion rates. Therefore, their conclusion was that optimal vitamin D may help up-regulate the systems needed to protect against URTI.
Some limitations of this study include participants started at adequate levels of vitamin D and therefore the changes might underestimate the importance of vitamin D’s effect on immunity and bigger changes might be seen when vitamin D levels start at an inadequate/deficient level. Another limitation to this study is they did not record incidents of URTI and therefore no conclusion could be made as to whether the immunological changes resulted in decreased illness.
Main points:
Research has clearly demonstrated that vitamin D is of critical importance in the bodies immune system however there is more to learn about how vitamin D levels impact the frequency of illness and severity, and at what level is the immune system compromised.
From the studies above we learn that:
- Optimal levels of vitamin D increase antibacterial peptides in the blood
- Optimal levels increase salivary IgA secretion rates and concentration
- Observational studies show that illness severity and length is decreased compared to lower levels of vitamin D.
Because salivary IgA is suppressed after intense exercise and taking vitamin D increases the IgA secretion rate and concentration, this may be one mechanism that optimal vitamin D is used in to protect against upper respiratory tract infections.
Practical application:
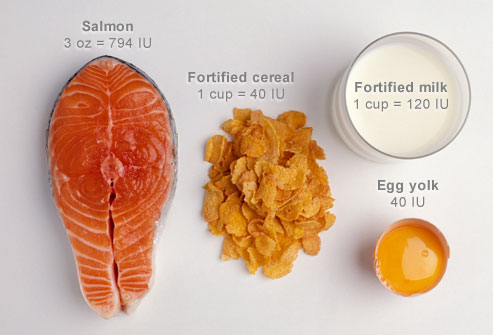
Should we be supplementing? Usually my belief is “food first, supplement second”. With that being said, there are few foods that contain high levels of vitamin D. We can make vitamin D from the sun, however we are too far north for adequate sun exposure to make vitamin D this time of year (fall through spring). Even in the summer we may make inadequate amounts of vitamin D from the sun if we wear sunscreen, have dark skin or train inside or early/later in the evening. It is likely a good idea to supplement to make sure you are getting adequate amounts of vitamin D. Not only does it play a role in immunity, but it also helps maintain bone and muscle health, and therefore it is an important nutrient.
How much vitamin D: Health Canada has set the Adequate Intake (AI) level of vitamin D at 600 International Units (IU)/day and the upper limit at 4000 IU/day for most ages with some exceptions. First AI means that there is not sufficient evidence to set a Recommended Dietary Allowance (set to meet the needs of 97-98% of healthy individuals) but the AI is assumed to be adequate. There is debate about the AI for vitamin D as many think this AI is set too low, and people are also supplementing over the upper limit (like in study 3 from above). In the following years this AI could see and increase.
Food Sources: People often think milk is the best source of vitamin D, however 1 cup of milk only provides around 100IU or 1/6 of your daily needs of vitamin D. One of the best sources is actually salmon, which, depending on the kind can provide anywhere between 200-600IU in one 2.5oz serving (the size of a deck of cards).
Supplements: Depending on diet and your current vitamin D status, supplementing with 1000-2000IU is should be enough to give your vitamin D levels a boost and is recommended, especially in the winter.
There are many other tactics athletes can try to maintain and help with increased immune function. If you would like to learn more, book an appointment so we can optimize your nutrition intake to support your health, wellbeing and athletic performance!
Related Article: Does Vitamin C help to prevent the common cold? Check out Dr. Delanghe’s past article.
Reference:
Nieman, D.C. Exercise effects on systemic immunity. Immunology and Cell Biology. 2000. 78: 496-501.
Gleeson, M. Immunological aspects of sport nutrition. Immunology and Cell Biology. 2016. 94: 117-123.
He, C.S., Handzlik, M., Fraser, W.D., Muhamad, A., Preston, H., Richardson, A., Gleeson, M. Influence of vitamin D status on respiratory infection incidence and immune function during 4 months of winter training in endurance sport athletes. Exerc Immunol Rev. 2013. 19: 86–101.
Li-Ng M., Aloia, J.F., Pollack, S., Cunha B.A., Mikhail, M., Yeh, J., & Berbari N. A randomized controlled trial of Vitamin D3 Supplementation for the prevention of symptomatic upper respiratory tract infections. Epidemiol. Infect. 2009. 137: 1396-1404.
He, C.S., Fraser, W.D., Tang, J., Brown, K., Renwich, S., Rudland-Thomas, J., Teah, J., Tanqueray E., & Gleeson. M. The effects of 14 weeks of vitamin D3 supplementation on antimicrobial peptides and proteins in athletes. Journal of Sports Sciences. 2016. 34: 67-74.


 Signs/Symptoms
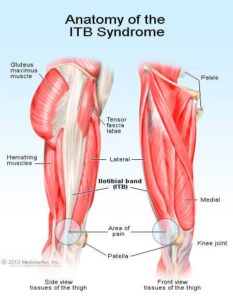
Signs/Symptoms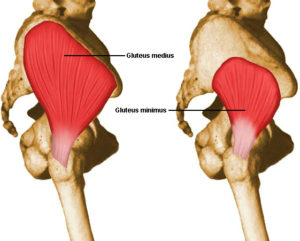 hip adduction angles during the stance phase of running (when the foot is in contact with the ground) compared to healthy controls.
hip adduction angles during the stance phase of running (when the foot is in contact with the ground) compared to healthy controls.

 It’s a topic I wrote about briefly in the past, but this week I wanted to take a closer look at things. Two strategies I discussed before were (1) getting acclimated to the heat and (2) pre-cooling.
It’s a topic I wrote about briefly in the past, but this week I wanted to take a closer look at things. Two strategies I discussed before were (1) getting acclimated to the heat and (2) pre-cooling.
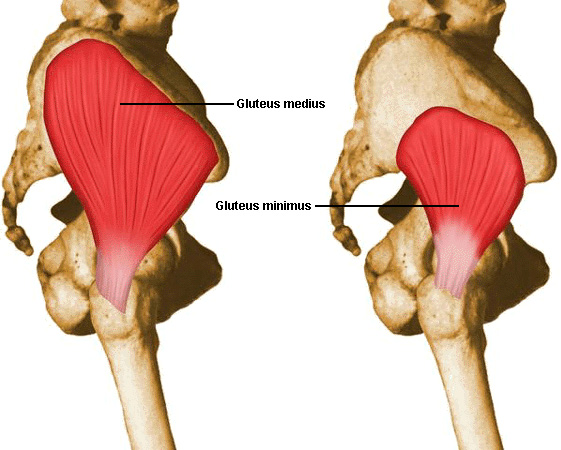
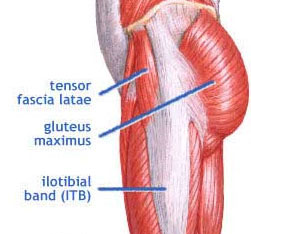
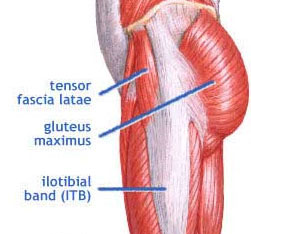
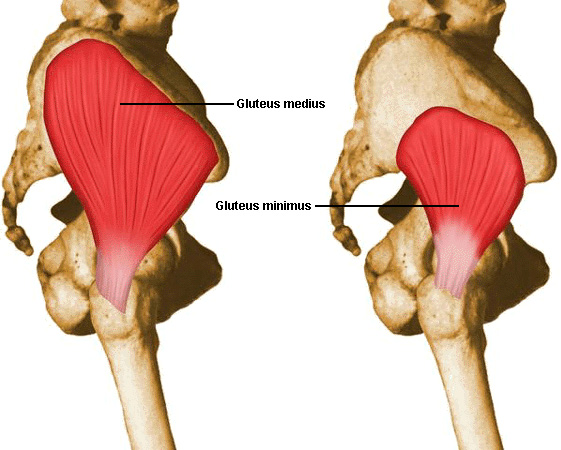 ed), gluteus maximus (GMax), gluteus minimus (GMin) and TFL (tensor fascia latae). The focus of this article is going to be on the gluteus medius because of its important role in stabilizing the pelvis.
ed), gluteus maximus (GMax), gluteus minimus (GMin) and TFL (tensor fascia latae). The focus of this article is going to be on the gluteus medius because of its important role in stabilizing the pelvis.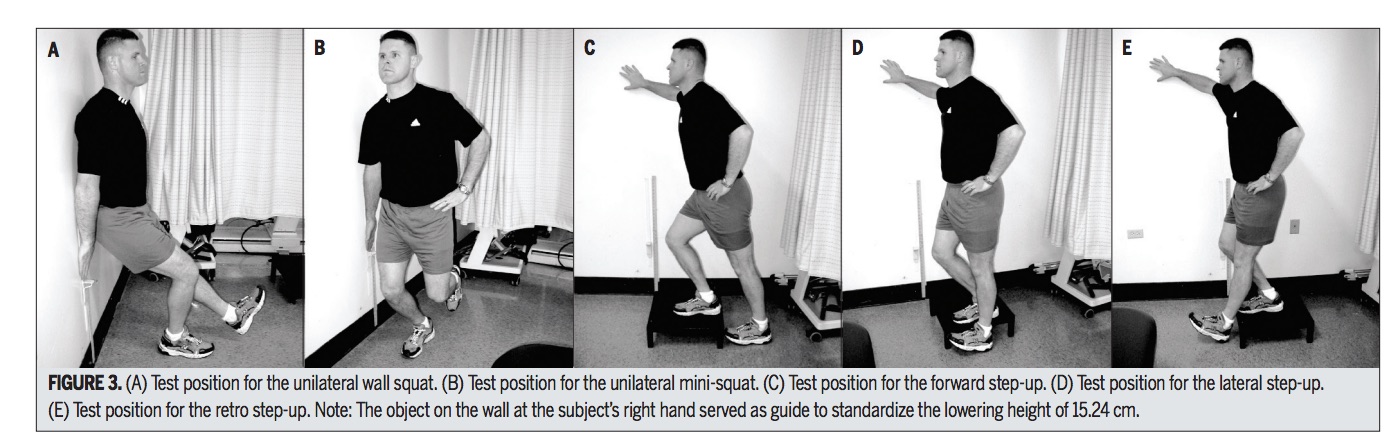
 Study #3: What happens when the gluts are weak?
Study #3: What happens when the gluts are weak?
 munology notes yet again to relearn what I already know (it’s always fun picturing the T-cells destroying the bad stuff). Times like these also motivate me to relearn other things, like how nothing gets rid of a cold other than some basics including: sufficient rest, fluids, stress management and a good diet.
munology notes yet again to relearn what I already know (it’s always fun picturing the T-cells destroying the bad stuff). Times like these also motivate me to relearn other things, like how nothing gets rid of a cold other than some basics including: sufficient rest, fluids, stress management and a good diet.