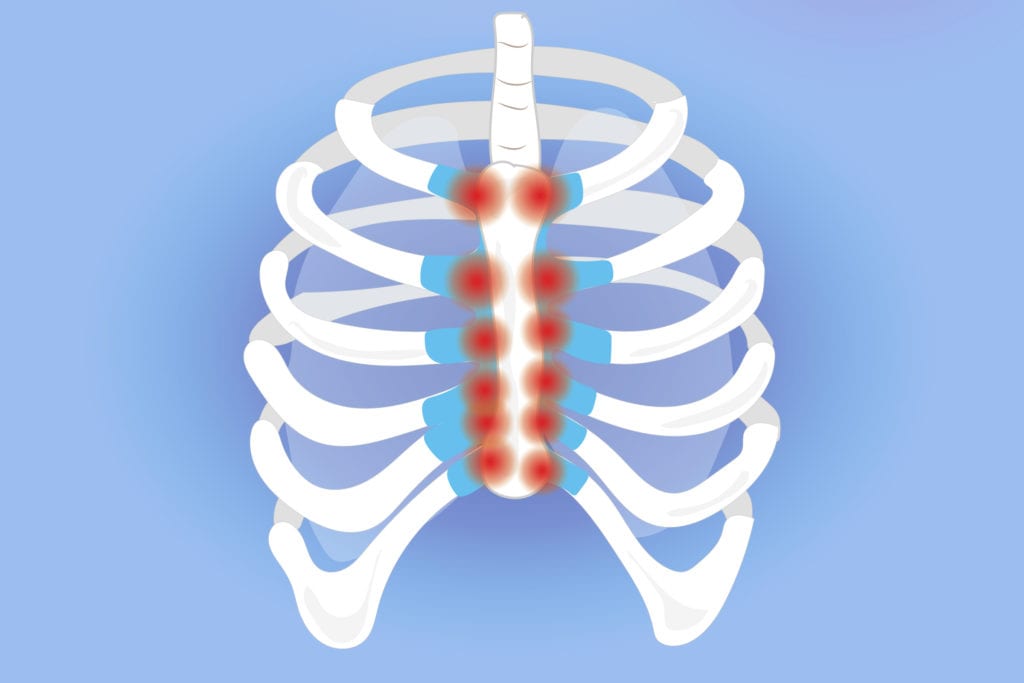
Your heart is fine, but your chest hurts? It could be costochondritis!
What is costochondritis?
Costochondritis is inflammation of the cartilage where the ribs attach to the sternum. It causes localized chest wall pain that can mimic heart-related pain but is not caused by cardiac disease. This summary takes an in-depth look at the most up to date research regarding this condition.
It is considered one of the more common musculoskeletal causes of chest pain and may account for up to about 30 percent of noncardiac chest pain cases seen in some clinical settings.
Clinical presentation
-Pain is usually localized and reproducible with palpation over the affected costosternal or costochondral joints.
-The pain may be sharp or aching.
– Symptoms often worsen with movement, deep breathing, or pressure on the chest wall.
– There is usually no visible swelling, redness, or systemic symptoms such as fever.
Diagnosis
– There is no specific laboratory test or imaging study that confirms costochondritis.
– Diagnosis is clinical and based primarily on history and physical examination.
– A key diagnostic feature is reproduction of pain with palpation of the anterior chest wall.
– Cardiac and other serious causes must first be excluded, especially in higher-risk patients.
Management
– Initial treatment is conservative and may include:
Analgesics such as acetaminophen and Nonsteroidal anti-inflammatory drugs (talk do your doctor!)
– Relative rest and activity modification is key. Complete rest isn’t good, but continuing with the activities that aggravate the condition do not allow for it heal!
Physiotherapy is also a crucial part of the management of this condition. Some examples include:
- Stretching and mobility exercises
These focus on improving chest wall and thoracic spine mobility.- Examples include:
Pectoral stretching, such as doorway stretches
Thoracic extension and mobility exercises
Breathing-based mobility drills to reduce rib cage stiffness
- Examples include:
- Manual therapy
- Performed by trained clinicians, this may include:
- Soft tissue mobilization of the chest wall and surrounding musculature
- Joint mobilization of the ribs and thoracic spine
- Trigger point release and myofascial techniques
- Rib mobilization techniques to normalize movement
Some small clinical studies and case series suggest that combining manual therapy with therapeutic exercise can reduce pain and improve function the most, but as always more research is needed!
Main takeaway
Costochondritis is an important and relatively common cause of noncardiac chest pain. It is diagnosed clinically after ruling out more serious co
nditions. Management is usually conservative and may include medication, rest, and targeted physical therapy interventions aimed at improving chest wall mobility, posture, and muscle function.
If you have questions about your pain, feel free to contact one of our Waterloo based chiropractors or physiotherapists, or book online HERE.